Table of Contents
Toggle- What Is Medication Reconciliation?
- Why Is Medication Reconciliation Important?
- When Does Medication Reconciliation Happen?
- Steps in the Medication Reconciliation Process
- Who Performs Medication Reconciliation?
- Challenges in Medication Reconciliation
- How Patients and Caregivers Can Help
- Benefits of Medication Reconciliation
- Conclusion
- Frequently Asked Questions (FAQs)
Healthcare can sometimes feel overwhelming, especially when it comes to managing multiple medications. If you’ve ever switched doctors, been admitted to a hospital, or cared for a loved one with several prescriptions, you know how confusing medication lists can get. That’s where medication reconciliation comes in.
This process is designed to improve patient safety, reduce medication errors, and ensure that every healthcare provider involved in a patient’s care has the same accurate information about their medicines.
In this blog, we’ll explore what medication reconciliation is, why it matters, how it works, and what patients and caregivers need to know.
What Is Medication Reconciliation?
Medication reconciliation is the process of creating the most accurate list possible of all the medications a patient is currently taking. This includes:
- Prescription drugs
- Over-the-counter (OTC) medications
- Herbal supplements
- Vitamins
The purpose is to compare this list against new prescriptions or treatment plans to avoid errors such as duplications, omissions, interactions, or incorrect doses.
In simple terms: It’s about making sure every healthcare provider knows exactly what medications a patient takes so that nothing important is missed or duplicated.
Why Is Medication Reconciliation Important?
Medication errors are one of the leading causes of preventable harm in healthcare. According to research, thousands of hospitalizations occur every year due to drug-related mistakes.
Key reasons why medication reconciliation is important:
- Prevents medication errors
- Avoids situations where a patient might accidentally be prescribed a drug they are already taking or one that interacts with another.
- Avoids situations where a patient might accidentally be prescribed a drug they are already taking or one that interacts with another.
- Improves patient safety
- Ensures correct dosages and avoids harmful side effects.
- Ensures correct dosages and avoids harmful side effects.
- Smooth transitions of care
- Especially critical when a patient moves from hospital to home, or from one doctor to another.
- Especially critical when a patient moves from hospital to home, or from one doctor to another.
- Encourages communication
- Patients, caregivers, pharmacists, and doctors all stay on the same page.
- Patients, caregivers, pharmacists, and doctors all stay on the same page.
- Reduces hospital readmissions
- Accurate medication records help patients recover safely at home without preventable complications.
When Does Medication Reconciliation Happen?
Medication reconciliation should occur whenever a patient’s care transitions from one setting to another. Common situations include:
- Hospital admission – Reviewing what the patient was taking before arriving.
- Transfers within a hospital – For example, moving from surgery to intensive care.
- Discharge from hospital – Ensuring patients leave with the right prescriptions.
- Doctor visits – Especially when seeing a new provider or specialist.
- Pharmacy consultations – Reviewing all medicines for accuracy and safety.

Steps in the Medication Reconciliation Process
Medication reconciliation is not just a quick check—it’s a step-by-step process carried out by healthcare professionals.
1. Collecting a complete medication history
- Patients or caregivers provide a list of all medications, including prescriptions, OTC drugs, supplements, and vitamins.
2. Verification
- Pharmacists, nurses, or doctors verify the accuracy by checking dosages, timing, and purpose of each medication.
3. Comparison
- The current list is compared with new prescriptions to identify differences, duplications, or potential drug interactions.
4. Correction
- Any errors or discrepancies are resolved in consultation with the patient and healthcare team.
5. Documentation and communication
- The final, reconciled list is documented and shared with all relevant healthcare providers.
Who Performs Medication Reconciliation?
Medication reconciliation is usually a team effort, involving:
- Doctors – Review and approve medication changes.
- Pharmacists – Play a key role in identifying drug interactions or duplications.
- Nurses – Help gather patient information and confirm details.
- Patients and caregivers – Provide firsthand knowledge of actual medication use.
Challenges in Medication Reconciliation
Even though it’s an essential safety practice, medication reconciliation can be challenging.
- Incomplete information – Patients may forget to mention supplements or OTC medications.
- Multiple prescribers – Different doctors may prescribe different medicines without full coordination.
- Poor communication – Between hospital staff, primary care providers, and pharmacists.
- Time constraints – Busy healthcare environments sometimes rush through reconciliation.
Despite these challenges, when done correctly, medication reconciliation significantly reduces the risk of errors.
How Patients and Caregivers Can Help
Medication reconciliation is most effective when patients and caregivers are actively involved. Here’s how you can help:
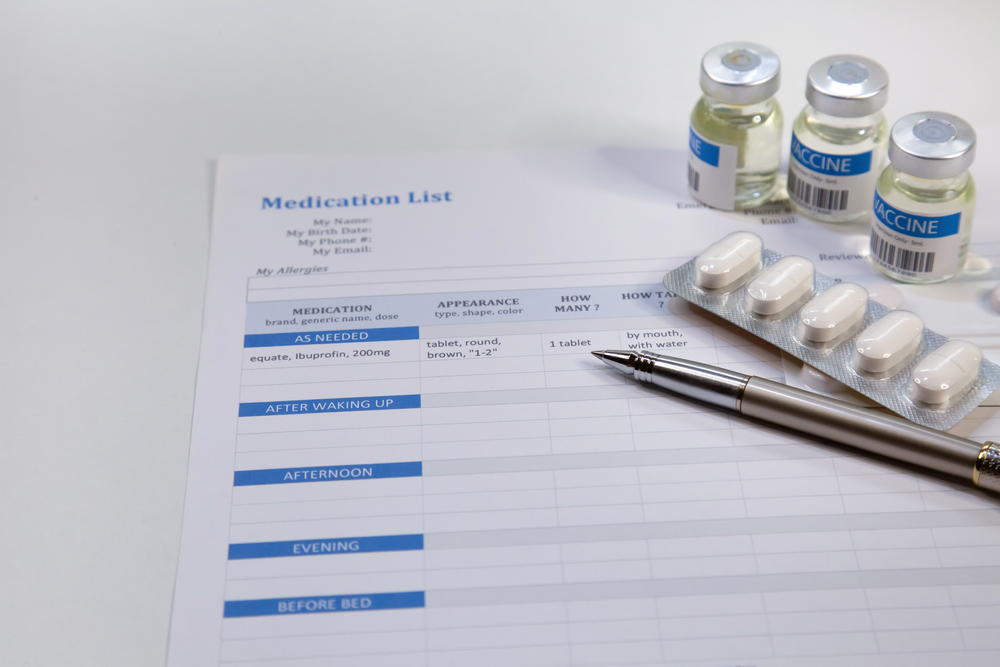
- Keep an updated medication list – Write down drug names, doses, frequency, and reasons for taking them.
- Bring medications to appointments – Carry actual medicine bottles or packaging.
- Ask questions – Don’t hesitate to clarify why a medicine is prescribed and whether it interacts with others.
- Update after changes – If a doctor stops or adds a medicine, update your list immediately.
- Share with all providers – Make sure every doctor, nurse, and pharmacist has the same list.
Benefits of Medication Reconciliation
- Reduces adverse drug events (ADEs).
- Promotes better patient outcomes.
- Improves trust between patients and providers.
- Saves healthcare costs by avoiding preventable hospital visits.
Conclusion
So, what is medication reconciliation? It’s a crucial process that ensures every patient’s medication list is accurate, complete, and safe. By preventing errors, reducing hospital readmissions, and improving communication, medication reconciliation plays a vital role in patient safety and quality healthcare.
Whether you’re a patient, caregiver, or healthcare provider, understanding this process can make a huge difference. Always keep your medication records up to date, share them with your care team, and ask questions when in doubt.
Medication reconciliation isn’t just a medical checklist—it’s a safeguard for your health and peace of mind.

Frequently Asked Questions (FAQs)
1. What is the goal of medication reconciliation?
The goal is to ensure patients receive the correct medications in the right dose at every point in their care.
2. Who is responsible for medication reconciliation?
It is a shared responsibility among doctors, pharmacists, nurses, and patients.
3. Is medication reconciliation only for hospital patients?
No. It should be done in hospitals, clinics, pharmacies, nursing homes, and even during routine doctor visits.
4. Can medication reconciliation prevent drug interactions?
Yes. By comparing all current medications, healthcare providers can identify and prevent harmful interactions.
5. How often should I update my medication list?
Every time there is a change—new prescription, dosage adjustment, or stopping a medicine.






